JavaScript is disabled for your browser. Some features of this site may not work without it.
Buscar en RiuNet
Listar
Mi cuenta
Estadísticas
Ayuda RiuNet
Admin. UPV
Cardiac action potential repolarization revisited: early repolarization shows all-or-none behaviour
Mostrar el registro sencillo del ítem
Ficheros en el ítem
| dc.contributor.author | Trenor Gomis, Beatriz Ana
|
es_ES |
| dc.contributor.author | Cardona-Urrego, Karen Eliana
|
es_ES |
| dc.contributor.author | Saiz Rodríguez, Francisco Javier
|
es_ES |
| dc.contributor.author | Noble, Denis
|
es_ES |
| dc.contributor.author | Giles, Wayne
|
es_ES |
| dc.date.accessioned | 2020-10-29T04:32:04Z | |
| dc.date.available | 2020-10-29T04:32:04Z | |
| dc.date.issued | 2017-11-01 | es_ES |
| dc.identifier.issn | 0022-3751 | es_ES |
| dc.identifier.uri | http://hdl.handle.net/10251/153463 | |
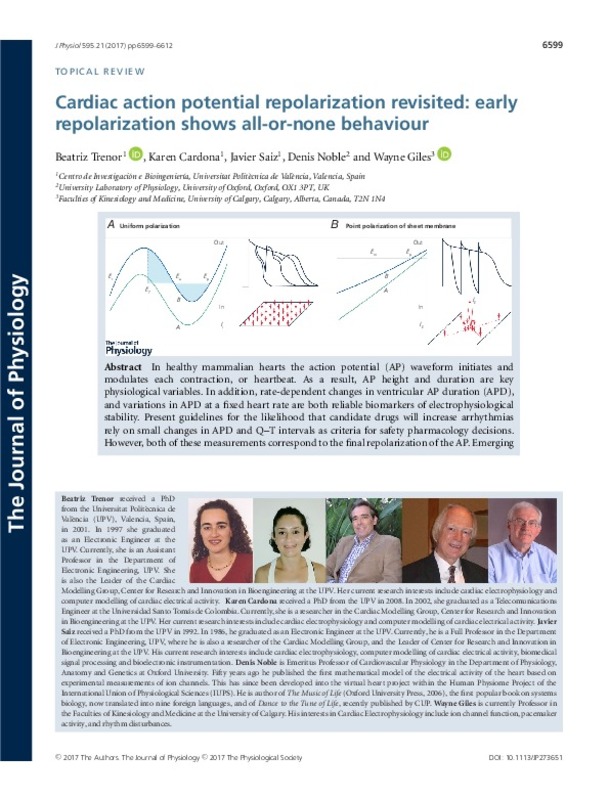
| dc.description.abstract | [EN] In healthy mammalian hearts the action potential (AP) waveform initiates and modulates each contraction, or heartbeat. As a result, AP height and duration are key physiological variables. In addition, rate-dependent changes in ventricular AP duration (APD), and variations in APD at a fixed heart rate are both reliable biomarkers of electrophysiological stability. Present guidelines for the likelihood that candidate drugs will increase arrhythmias rely on small changes in APD and Q-T intervals as criteria for safety pharmacology decisions. However, both of these measurements correspond to the final repolarization of the AP. Emerging clinical evidence draws attention to the early repolarization phase of the action potential (and the J-wave of the ECG) as an additional important biomarker for arrhythmogenesis. Here we provide a mechanistic background to this early repolarization syndrome by summarizing the evidence that both the initial depolarization and repolarization phases of the cardiac action potential can exhibit distinct time- and voltage-dependent thresholds, and also demonstrating that both can show regenerative all-or-none behaviour. An important consequence of this is that not all of the dynamics of action potential repolarization in human ventricle can be captured by data from single myocytes when these results are expressed as repolarization reserve'. For example, the complex pattern of cell-to-cell current flow that is responsible for AP conduction (propagation) within the mammalian myocardium can change APD and the Q-T interval of the electrocardiogram alter APD stability, and modulate responsiveness to pharmacological agents (such as Class III anti-arrhythmic drugs). | es_ES |
| dc.description.sponsorship | The Giles Laboratory acknowledges funding from the Canadian Institutes for Health Research. The computational work in Spain, was funded from the Ministerio de Economia, Industria y Competitividad of Spain (DPI2016-75799-R) and AEI/FEDER, UE, and the Programa Prometeu (PROMETEU/2016/088) de la Conselleria d'Educacio, Formacio/Ocupacio, Generalitat Valenciana | es_ES |
| dc.language | Inglés | es_ES |
| dc.publisher | Blackwell Publishing | es_ES |
| dc.relation.ispartof | The Journal of Physiology | es_ES |
| dc.rights | Reserva de todos los derechos | es_ES |
| dc.subject.classification | TECNOLOGIA ELECTRONICA | es_ES |
| dc.title | Cardiac action potential repolarization revisited: early repolarization shows all-or-none behaviour | es_ES |
| dc.type | Artículo | es_ES |
| dc.identifier.doi | 10.1113/JP273651 | es_ES |
| dc.relation.projectID | info:eu-repo/grantAgreement/GVA//PROMETEO%2F2016%2F088/ES/MODELOS COMPUTACIONALES PERSONALIZADOS MULTI-ESCALA PARA LA OPTIMIZACION DEL DIAGNOSTICO Y TRATAMIENTO DE ARRITMIAS CARDIACAS (PERSONALISED DIGITAL HEART)/ | es_ES |
| dc.relation.projectID | info:eu-repo/grantAgreement/MINECO//DPI2016-75799-R/ES/TECNOLOGIAS COMPUTACIONALES PARA LA OPTIMIZACION DE TERAPIAS PERSONALIZADAS DE PATOLOGIAS AURICULARES Y VENTRICULARES/ | es_ES |
| dc.rights.accessRights | Abierto | es_ES |
| dc.contributor.affiliation | Universitat Politècnica de València. Departamento de Ingeniería Electrónica - Departament d'Enginyeria Electrònica | es_ES |
| dc.description.bibliographicCitation | Trenor Gomis, BA.; Cardona-Urrego, KE.; Saiz Rodríguez, FJ.; Noble, D.; Giles, W. (2017). Cardiac action potential repolarization revisited: early repolarization shows all-or-none behaviour. The Journal of Physiology. 595(21):6599-6612. https://doi.org/10.1113/JP273651 | es_ES |
| dc.description.accrualMethod | S | es_ES |
| dc.relation.publisherversion | https://doi.org/10.1113/JP273651 | es_ES |
| dc.description.upvformatpinicio | 6599 | es_ES |
| dc.description.upvformatpfin | 6612 | es_ES |
| dc.type.version | info:eu-repo/semantics/publishedVersion | es_ES |
| dc.description.volume | 595 | es_ES |
| dc.description.issue | 21 | es_ES |
| dc.identifier.pmid | 28815597 | es_ES |
| dc.identifier.pmcid | PMC5663823 | es_ES |
| dc.relation.pasarela | S\343941 | es_ES |
| dc.contributor.funder | Generalitat Valenciana | es_ES |
| dc.contributor.funder | Agencia Estatal de Investigación | es_ES |
| dc.description.references | Anderson, M. E., Al-Khatib, S. M., Roden, D. M., & Califf, R. M. (2002). Cardiac repolarization: Current knowledge, critical gaps, and new approaches to drug development and patient management. American Heart Journal, 144(5), 769-781. doi:10.1067/mhj.2002.125804 | es_ES |
| dc.description.references | ANTZELEVITCH, C. (2005). Modulation of Transmural Repolarization. Annals of the New York Academy of Sciences, 1047(1), 314-323. doi:10.1196/annals.1341.028 | es_ES |
| dc.description.references | Antzelevitch, C. (2012). Genetic, Molecular and Cellular Mechanisms Underlying the J Wave Syndromes. Circulation Journal, 76(5), 1054-1065. doi:10.1253/circj.cj-12-0284 | es_ES |
| dc.description.references | Antzelevitch, C., & Yan, G.-X. (2010). J wave syndromes. Heart Rhythm, 7(4), 549-558. doi:10.1016/j.hrthm.2009.12.006 | es_ES |
| dc.description.references | Antzelevitch, C., Yan, G.-X., & Viskin, S. (2011). Rationale for the Use of the Terms J-Wave Syndromes and Early Repolarization. Journal of the American College of Cardiology, 57(15), 1587-1590. doi:10.1016/j.jacc.2010.11.038 | es_ES |
| dc.description.references | Ballou, L. M., Lin, R. Z., & Cohen, I. S. (2015). Control of Cardiac Repolarization by Phosphoinositide 3-Kinase Signaling to Ion Channels. Circulation Research, 116(1), 127-137. doi:10.1161/circresaha.116.303975 | es_ES |
| dc.description.references | Bean, B. P. (2007). The action potential in mammalian central neurons. Nature Reviews Neuroscience, 8(6), 451-465. doi:10.1038/nrn2148 | es_ES |
| dc.description.references | Belardinelli, L., Giles, W. R., Rajamani, S., Karagueuzian, H. S., & Shryock, J. C. (2015). Cardiac late Na+ current: Proarrhythmic effects, roles in long QT syndromes, and pathological relationship to CaMKII and oxidative stress. Heart Rhythm, 12(2), 440-448. doi:10.1016/j.hrthm.2014.11.009 | es_ES |
| dc.description.references | Bondarenko, V. E., & Rasmusson, R. L. (2010). Transmural heterogeneity of repolarization and Ca2+ handling in a model of mouse ventricular tissue. American Journal of Physiology-Heart and Circulatory Physiology, 299(2), H454-H469. doi:10.1152/ajpheart.00907.2009 | es_ES |
| dc.description.references | Bouchard, R. A., Clark, R. B., & Giles, W. R. (1995). Effects of Action Potential Duration on Excitation-Contraction Coupling in Rat Ventricular Myocytes. Circulation Research, 76(5), 790-801. doi:10.1161/01.res.76.5.790 | es_ES |
| dc.description.references | Bouchard, R., Clark, R. B., Juhasz, A. E., & Giles, W. R. (2004). Changes in extracellular K+concentration modulate contractility of rat and rabbit cardiac myocytes via the inward rectifier K+currentIK1. The Journal of Physiology, 556(3), 773-790. doi:10.1113/jphysiol.2003.058248 | es_ES |
| dc.description.references | Bowes, J., Brown, A. J., Hamon, J., Jarolimek, W., Sridhar, A., Waldron, G., & Whitebread, S. (2012). Reducing safety-related drug attrition: the use of in vitro pharmacological profiling. Nature Reviews Drug Discovery, 11(12), 909-922. doi:10.1038/nrd3845 | es_ES |
| dc.description.references | Burashnikov, E., Pfeiffer, R., Barajas-Martinez, H., Delpón, E., Hu, D., Desai, M., … Antzelevitch, C. (2010). Mutations in the cardiac L-type calcium channel associated with inherited J-wave syndromes and sudden cardiac death. Heart Rhythm, 7(12), 1872-1882. doi:10.1016/j.hrthm.2010.08.026 | es_ES |
| dc.description.references | Chandler, W. K., & Meves, H. (1970). Evidence for two types of sodium conductance in axons perfused with sodium fluoride solution. The Journal of Physiology, 211(3), 653-678. doi:10.1113/jphysiol.1970.sp009298 | es_ES |
| dc.description.references | Chandler, W. K., & Meves, H. (1970). Slow changes in membrane permeability and long-lasting action potentials in axons perfused with fluoride solutions. The Journal of Physiology, 211(3), 707-728. doi:10.1113/jphysiol.1970.sp009300 | es_ES |
| dc.description.references | Chi, K. R. (2013). Revolution dawning in cardiotoxicity testing. Nature Reviews Drug Discovery, 12(8), 565-567. doi:10.1038/nrd4083 | es_ES |
| dc.description.references | CLARK, R. B., BOUCHARD, R. A., & GILES, W. R. (1996). Action Potential Duration Modulates Calcium Influx, Na+-Ca2+ Exchange, and Intracellular Calcium Release in Rat Ventricular Myocytesa. Annals of the New York Academy of Sciences, 779(1), 417-429. doi:10.1111/j.1749-6632.1996.tb44817.x | es_ES |
| dc.description.references | Clark, R. B., Tremblay, A., Melnyk, P., Allen, B. G., Giles, W. R., & Fiset, C. (2001). T-tubule localization of the inward-rectifier K+ channel in mouse ventricular myocytes: a role in K+ accumulation. The Journal of Physiology, 537(3), 979-992. doi:10.1113/jphysiol.2001.012708 | es_ES |
| dc.description.references | Coronel, R., Wilders, R., Verkerk, A. O., Wiegerinck, R. F., Benoist, D., & Bernus, O. (2013). Electrophysiological changes in heart failure and their implications for arrhythmogenesis. Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease, 1832(12), 2432-2441. doi:10.1016/j.bbadis.2013.04.002 | es_ES |
| dc.description.references | Cranefield, P. F., & Hoffman, B. F. (1958). PROPAGATED REPOLARIZATION IN HEART MUSCLE. Journal of General Physiology, 41(4), 633-649. doi:10.1085/jgp.41.4.633 | es_ES |
| dc.description.references | Fink, M., Giles, W. R., & Noble, D. (2006). Contributions of inwardly rectifying K + currents to repolarization assessed using mathematical models of human ventricular myocytes. Philosophical Transactions of the Royal Society A: Mathematical, Physical and Engineering Sciences, 364(1842), 1207-1222. doi:10.1098/rsta.2006.1765 | es_ES |
| dc.description.references | Giebisch, G., & Weidmann, S. (1971). Membrane Currents in Mammalian Ventricular Heart Muscle Fibers Using a Voltage-Clamp Technique. Journal of General Physiology, 57(3), 290-296. doi:10.1085/jgp.57.3.290 | es_ES |
| dc.description.references | Gray, R. A., Mashburn, D. N., Sidorov, V. Y., & Wikswo, J. P. (2013). Quantification of Transmembrane Currents during Action Potential Propagation in the Heart. Biophysical Journal, 104(1), 268-278. doi:10.1016/j.bpj.2012.11.007 | es_ES |
| dc.description.references | Gussak, I., & Antzelevitch, C. (2000). Early repolarization syndrome: Clinical characteristics and possible cellular and ionic mechanisms. Journal of Electrocardiology, 33(4), 299-309. doi:10.1054/jelc.2000.18106 | es_ES |
| dc.description.references | Gussak, I., Antzelevitch, C., Hammill, S. C., Shen, W. K., & Bjerregaard, P. (2003). Cardiac Repolarization. doi:10.1385/1592593623 | es_ES |
| dc.description.references | Haïssaguerre, M., Derval, N., Sacher, F., Jesel, L., Deisenhofer, I., de Roy, L., … Clémenty, J. (2008). Sudden Cardiac Arrest Associated with Early Repolarization. New England Journal of Medicine, 358(19), 2016-2023. doi:10.1056/nejmoa071968 | es_ES |
| dc.description.references | HALL, A. E., & NOBLE, D. (1963). Transient Responses of Purkinje Fibres to Non-uniform Currents. Nature, 199(4900), 1294-1295. doi:10.1038/1991294a0 | es_ES |
| dc.description.references | Hoogendijk, M. G., Potse, M., & Coronel, R. (2012). Early repolarization patterns: The good, the bad, and the ugly? Heart Rhythm, 9(2), 230-231. doi:10.1016/j.hrthm.2011.09.064 | es_ES |
| dc.description.references | Hoogendijk, M. G., Potse, M., & Coronel, R. (2013). Critical appraisal of the mechanism underlying J waves. Journal of Electrocardiology, 46(5), 390-394. doi:10.1016/j.jelectrocard.2013.06.017 | es_ES |
| dc.description.references | Huxley, A. F. (1959). ION MOVEMENTS DURING NERVE ACTIVITY. Annals of the New York Academy of Sciences, 81(2), 221-246. doi:10.1111/j.1749-6632.1959.tb49311.x | es_ES |
| dc.description.references | Janse, M. (2004). Electrophysiological changes in heart failure and their relationship to arrhythmogenesis. Cardiovascular Research, 61(2), 208-217. doi:10.1016/j.cardiores.2003.11.018 | es_ES |
| dc.description.references | Jost, N., Virág, L., Comtois, P., Ördög, B., Szuts, V., Seprényi, G., … Nattel, S. (2013). Ionic mechanisms limiting cardiac repolarization reserve in humans compared to dogs. The Journal of Physiology, 591(17), 4189-4206. doi:10.1113/jphysiol.2013.261198 | es_ES |
| dc.description.references | Kannankeril, P., Roden, D. M., & Darbar, D. (2010). Drug-Induced Long QT Syndrome. Pharmacological Reviews, 62(4), 760-781. doi:10.1124/pr.110.003723 | es_ES |
| dc.description.references | Kelly, A., Ghouri, I. A., Kemi, O. J., Bishop, M. J., Bernus, O., Fenton, F. H., … Smith, G. L. (2013). Subepicardial Action Potential Characteristics Are a Function of Depth and Activation Sequence in Isolated Rabbit Hearts. Circulation: Arrhythmia and Electrophysiology, 6(4), 809-817. doi:10.1161/circep.113.000334 | es_ES |
| dc.description.references | Kondo, R. P., Dederko, D. A., Teutsch, C., Chrast, J., Catalucci, D., Chien, K. R., & Giles, W. R. (2006). Comparison of contraction and calcium handling between right and left ventricular myocytes from adult mouse heart: a role for repolarization waveform. The Journal of Physiology, 571(1), 131-146. doi:10.1113/jphysiol.2005.101428 | es_ES |
| dc.description.references | Kramer, J., Obejero-Paz, C. A., Myatt, G., Kuryshev, Y. A., Bruening-Wright, A., Verducci, J. S., & Brown, A. M. (2013). MICE Models: Superior to the HERG Model in Predicting Torsade de Pointes. Scientific Reports, 3(1). doi:10.1038/srep02100 | es_ES |
| dc.description.references | Libbus, I., Wan, X., & Rosenbaum, D. S. (2004). Electrotonic load triggers remodeling of repolarizing current Ito in ventricle. American Journal of Physiology-Heart and Circulatory Physiology, 286(5), H1901-H1909. doi:10.1152/ajpheart.00581.2003 | es_ES |
| dc.description.references | Liu, M. B., Ko, C. Y., Song, Z., Garfinkel, A., Weiss, J. N., & Qu, Z. (2016). A Dynamical Threshold for Cardiac Delayed Afterdepolarization-Mediated Triggered Activity. Biophysical Journal, 111(11), 2523-2533. doi:10.1016/j.bpj.2016.10.009 | es_ES |
| dc.description.references | Macfarlane, P. W., Antzelevitch, C., Haissaguerre, M., Huikuri, H. V., Potse, M., Rosso, R., … Yan, G.-X. (2015). The Early Repolarization Pattern. Journal of the American College of Cardiology, 66(4), 470-477. doi:10.1016/j.jacc.2015.05.033 | es_ES |
| dc.description.references | Mirams, G. R., Davies, M. R., Cui, Y., Kohl, P., & Noble, D. (2012). Application of cardiac electrophysiology simulations to pro‐arrhythmic safety testing. British Journal of Pharmacology, 167(5), 932-945. doi:10.1111/j.1476-5381.2012.02020.x | es_ES |
| dc.description.references | Mirams, G. R., Pathmanathan, P., Gray, R. A., Challenor, P., & Clayton, R. H. (2016). Uncertainty and variability in computational and mathematical models of cardiac physiology. The Journal of Physiology, 594(23), 6833-6847. doi:10.1113/jp271671 | es_ES |
| dc.description.references | Mohri, S., Shimizu, J., Mika, Y., Shemer, I., Wang, J., Ben-Haim, S., & Burkhoff, D. (2003). Electric currents applied during refractory period enhance contractility and systolic calcium in the ferret heart. American Journal of Physiology-Heart and Circulatory Physiology, 284(4), H1119-H1123. doi:10.1152/ajpheart.00378.2002 | es_ES |
| dc.description.references | Moreno, J. D., Yang, P.-C., Bankston, J. R., Grandi, E., Bers, D. M., Kass, R. S., & Clancy, C. E. (2013). Ranolazine for Congenital and Acquired Late I Na -Linked Arrhythmias. Circulation Research, 113(7). doi:10.1161/circresaha.113.301971 | es_ES |
| dc.description.references | Myles, R. C., Bernus, O., Burton, F. L., Cobbe, S. M., & Smith, G. L. (2010). Effect of activation sequence on transmural patterns of repolarization and action potential duration in rabbit ventricular myocardium. American Journal of Physiology-Heart and Circulatory Physiology, 299(6), H1812-H1822. doi:10.1152/ajpheart.00518.2010 | es_ES |
| dc.description.references | Näbauer, M., Beuckelmann, D. J., & Erdmann, E. (1993). Characteristics of transient outward current in human ventricular myocytes from patients with terminal heart failure. Circulation Research, 73(2), 386-394. doi:10.1161/01.res.73.2.386 | es_ES |
| dc.description.references | Nattel, S. (2010). Sudden Cardio Arrest: When normal ECG variants turn lethal. Nature Medicine, 16(6), 646-647. doi:10.1038/nm0610-646 | es_ES |
| dc.description.references | Nerbonne, J. M., & Kass, R. S. (2005). Molecular Physiology of Cardiac Repolarization. Physiological Reviews, 85(4), 1205-1253. doi:10.1152/physrev.00002.2005 | es_ES |
| dc.description.references | NOBLE, D. (1960). Cardiac Action and Pacemaker Potentials based on the Hodgkin-Huxley Equations. Nature, 188(4749), 495-497. doi:10.1038/188495b0 | es_ES |
| dc.description.references | Noble, D. (1962). A modification of the Hodgkin-Huxley equations applicable to Purkinje fibre action and pacemaker potentials. The Journal of Physiology, 160(2), 317-352. doi:10.1113/jphysiol.1962.sp006849 | es_ES |
| dc.description.references | Noble, D. (1962). The Voltage Dependence of the Cardiac Membrane Conductance. Biophysical Journal, 2(5), 381-393. doi:10.1016/s0006-3495(62)86862-3 | es_ES |
| dc.description.references | Noble, D., & Tsien, R. W. (1972). The Repolarization Process of Heart Cells. Electrical Phenomena in the Heart, 133-161. doi:10.1016/b978-0-12-208950-3.50012-0 | es_ES |
| dc.description.references | O’Hara, T., Virág, L., Varró, A., & Rudy, Y. (2011). Simulation of the Undiseased Human Cardiac Ventricular Action Potential: Model Formulation and Experimental Validation. PLoS Computational Biology, 7(5), e1002061. doi:10.1371/journal.pcbi.1002061 | es_ES |
| dc.description.references | Osborn, J. J. (1953). Experimental Hypothermia: Respiratory and Blood ph Changes in Relation to Cardiac Function. American Journal of Physiology-Legacy Content, 175(3), 389-398. doi:10.1152/ajplegacy.1953.175.3.389 | es_ES |
| dc.description.references | Qu, Z., Xie, L.-H., Olcese, R., Karagueuzian, H. S., Chen, P.-S., Garfinkel, A., & Weiss, J. N. (2013). Early afterdepolarizations in cardiac myocytes: beyond reduced repolarization reserve. Cardiovascular Research, 99(1), 6-15. doi:10.1093/cvr/cvt104 | es_ES |
| dc.description.references | Reuter, H. (1973). Divalent cations as charge carriers in excitable membranes. Progress in Biophysics and Molecular Biology, 26, 1-43. doi:10.1016/0079-6107(73)90016-3 | es_ES |
| dc.description.references | Roden, D. M. (2004). Drug-Induced Prolongation of the QT Interval. New England Journal of Medicine, 350(10), 1013-1022. doi:10.1056/nejmra032426 | es_ES |
| dc.description.references | Roden, D. M. (2008). Repolarization Reserve. Circulation, 118(10), 981-982. doi:10.1161/circulationaha.108.798918 | es_ES |
| dc.description.references | Roden, D. M., & Abraham, R. L. (2011). Refining repolarization reserve. Heart Rhythm, 8(11), 1756-1757. doi:10.1016/j.hrthm.2011.06.024 | es_ES |
| dc.description.references | Roden, D. M., & Yang, T. (2005). Protecting the Heart Against Arrhythmias: Potassium Current Physiology and Repolarization Reserve. Circulation, 112(10), 1376-1378. doi:10.1161/circulationaha.105.562777 | es_ES |
| dc.description.references | Romero, L., Pueyo, E., Fink, M., & Rodríguez, B. (2009). Impact of ionic current variability on human ventricular cellular electrophysiology. American Journal of Physiology-Heart and Circulatory Physiology, 297(4), H1436-H1445. doi:10.1152/ajpheart.00263.2009 | es_ES |
| dc.description.references | Romero, L., Trenor, B., Yang, P.-C., Saiz, J., & Clancy, C. E. (2014). In silico screening of the impact of hERG channel kinetic abnormalities on channel block and susceptibility to acquired long QT syndrome. Journal of Molecular and Cellular Cardiology, 72, 126-137. doi:10.1016/j.yjmcc.2014.02.018 | es_ES |
| dc.description.references | Rosso, R., Adler, A., Halkin, A., & Viskin, S. (2011). Risk of sudden death among young individuals with J waves and early repolarization: Putting the evidence into perspective. Heart Rhythm, 8(6), 923-929. doi:10.1016/j.hrthm.2011.01.037 | es_ES |
| dc.description.references | Rosso, R., Glikson, E., Belhassen, B., Katz, A., Halkin, A., Steinvil, A., & Viskin, S. (2012). Distinguishing «benign» from «malignant early repolarization»: The value of the ST-segment morphology. Heart Rhythm, 9(2), 225-229. doi:10.1016/j.hrthm.2011.09.012 | es_ES |
| dc.description.references | Saegusa, N., Garg, V., & Spitzer, K. W. (2013). Modulation of ventricular transient outward K+ current by acidosis and its effects on excitation-contraction coupling. American Journal of Physiology-Heart and Circulatory Physiology, 304(12), H1680-H1696. doi:10.1152/ajpheart.00070.2013 | es_ES |
| dc.description.references | Sager, P. T., Gintant, G., Turner, J. R., Pettit, S., & Stockbridge, N. (2014). Rechanneling the cardiac proarrhythmia safety paradigm: A meeting report from the Cardiac Safety Research Consortium. American Heart Journal, 167(3), 292-300. doi:10.1016/j.ahj.2013.11.004 | es_ES |
| dc.description.references | Sah, R., Ramirez, R. J., Oudit, G. Y., Gidrewicz, D., Trivieri, M. G., Zobel, C., & Backx, P. H. (2003). Regulation of cardiac excitation-contraction coupling by action potential repolarization: role of the transient outward potassium current (Ito). The Journal of Physiology, 546(1), 5-18. doi:10.1113/jphysiol.2002.026468 | es_ES |
| dc.description.references | Sampson, K. J., & Henriquez, C. S. (2005). Electrotonic influences on action potential duration dispersion in small hearts: a simulation study. American Journal of Physiology-Heart and Circulatory Physiology, 289(1), H350-H360. doi:10.1152/ajpheart.00507.2004 | es_ES |
| dc.description.references | Sarkar, A. X., & Sobie, E. A. (2011). Quantification of repolarization reserve to understand interpatient variability in the response to proarrhythmic drugs: A computational analysis. Heart Rhythm, 8(11), 1749-1755. doi:10.1016/j.hrthm.2011.05.023 | es_ES |
| dc.description.references | Sarkar, A. X., Christini, D. J., & Sobie, E. A. (2012). Exploiting mathematical models to illuminate electrophysiological variability between individuals. The Journal of Physiology, 590(11), 2555-2567. doi:10.1113/jphysiol.2011.223313 | es_ES |
| dc.description.references | Silva, J., & Rudy, Y. (2005). Subunit Interaction Determines I Ks Participation in Cardiac Repolarization and Repolarization Reserve. Circulation, 112(10), 1384-1391. doi:10.1161/circulationaha.105.543306 | es_ES |
| dc.description.references | SPITZER, K. W., POLLARD, A. E., YANG, L., ZANIBONI, M., CORDEIRO, J. M., & HUELSING, D. J. (2006). Cell-to-Cell Electrical Interactions During Early and Late Repolarization. Journal of Cardiovascular Electrophysiology, 17(s1), S8-S14. doi:10.1111/j.1540-8167.2006.00379.x | es_ES |
| dc.description.references | Tadros, R., Ton, A.-T., Fiset, C., & Nattel, S. (2014). Sex Differences in Cardiac Electrophysiology and Clinical Arrhythmias: Epidemiology, Therapeutics, and Mechanisms. Canadian Journal of Cardiology, 30(7), 783-792. doi:10.1016/j.cjca.2014.03.032 | es_ES |
| dc.description.references | Taggart, P. (2001). Transmural repolarisation in the left ventricle in humans during normoxia and ischaemia. Cardiovascular Research, 50(3), 454-462. doi:10.1016/s0008-6363(01)00223-1 | es_ES |
| dc.description.references | Teutsch, C., Kondo, R. P., Dederko, D. A., Chrast, J., Chien, K. R., & Giles, W. R. (2007). Spatial distributions of Kv4 channels and KChip2 isoforms in the murine heart based on laser capture microdissection. Cardiovascular Research, 73(4), 739-749. doi:10.1016/j.cardiores.2006.11.034 | es_ES |
| dc.description.references | Tikkanen, J. T., Anttonen, O., Junttila, M. J., Aro, A. L., Kerola, T., Rissanen, H. A., … Huikuri, H. V. (2009). Long-Term Outcome Associated with Early Repolarization on Electrocardiography. New England Journal of Medicine, 361(26), 2529-2537. doi:10.1056/nejmoa0907589 | es_ES |
| dc.description.references | Thomsen, M. B. (2007). Double pharmacological challenge on repolarization opens new avenues for drug safety research. British Journal of Pharmacology, 151(7), 909-911. doi:10.1038/sj.bjp.0707299 | es_ES |
| dc.description.references | THOMSEN, M., OROS, A., SCHOENMAKERS, M., VANOPSTAL, J., MAAS, J., BEEKMAN, J., & VOS, M. (2007). Proarrhythmic electrical remodelling is associated with increased beat-to-beat variability of repolarisation. Cardiovascular Research, 73(3), 521-530. doi:10.1016/j.cardiores.2006.11.025 | es_ES |
| dc.description.references | Varkevisser, R., Wijers, S. C., van der Heyden, M. A. G., Beekman, J. D. M., Meine, M., & Vos, M. A. (2012). Beat-to-beat variability of repolarization as a new biomarker for proarrhythmia in vivo. Heart Rhythm, 9(10), 1718-1726. doi:10.1016/j.hrthm.2012.05.016 | es_ES |
| dc.description.references | Varró, A., & Baczkó, I. (2011). Cardiac ventricular repolarization reserve: a principle for understanding drug-related proarrhythmic risk. British Journal of Pharmacology, 164(1), 14-36. doi:10.1111/j.1476-5381.2011.01367.x | es_ES |
| dc.description.references | Vicente, J., Johannesen, L., Mason, J. W., Crumb, W. J., Pueyo, E., Stockbridge, N., & Strauss, D. G. (2015). Comprehensive T wave Morphology Assessment in a Randomized Clinical Study of Dofetilide, Quinidine, Ranolazine, and Verapamil. Journal of the American Heart Association, 4(4). doi:10.1161/jaha.114.001615 | es_ES |
| dc.description.references | Walmsley, J., Rodriguez, J. F., Mirams, G. R., Burrage, K., Efimov, I. R., & Rodriguez, B. (2013). mRNA Expression Levels in Failing Human Hearts Predict Cellular Electrophysiological Remodeling: A Population-Based Simulation Study. PLoS ONE, 8(2), e56359. doi:10.1371/journal.pone.0056359 | es_ES |
| dc.description.references | Wang, Y., Cheng, J., Joyner, R. W., Wagner, M. B., & Hill, J. A. (2006). Remodeling of Early-Phase Repolarization. Circulation, 113(15), 1849-1856. doi:10.1161/circulationaha.106.615682 | es_ES |
| dc.description.references | Weidmann, S. (1951). Effect of current flow on the membrane potential of cardiac muscle. The Journal of Physiology, 115(2), 227-236. doi:10.1113/jphysiol.1951.sp004667 | es_ES |
| dc.description.references | Weidmann, S. (1957). RESTING AND ACTION POTENTIALS OF CARDIAC MUSCLE. Annals of the New York Academy of Sciences, 65(6), 663-678. doi:10.1111/j.1749-6632.1957.tb36674.x | es_ES |
| dc.description.references | Wellens, H. J. (2008). Early Repolarization Revisited. New England Journal of Medicine, 358(19), 2063-2065. doi:10.1056/nejme0801060 | es_ES |
| dc.description.references | WOOD, E. H., HEPPNER, R. L., & WEIDMANN, S. (1969). Inotropic Effects of Electric Currents. Circulation Research, 24(3), 409-445. doi:10.1161/01.res.24.3.409 | es_ES |
| dc.description.references | Xiao, L., Xiao, J., Luo, X., Lin, H., Wang, Z., & Nattel, S. (2008). Feedback Remodeling of Cardiac Potassium Current Expression. Circulation, 118(10), 983-992. doi:10.1161/circulationaha.107.758672 | es_ES |
| dc.description.references | Xiao, L., Zhang, L., Han, W., Wang, Z., & Nattel, S. (2006). Sex-based transmural differences in cardiac repolarization and ionic-current properties in canine left ventricles. American Journal of Physiology-Heart and Circulatory Physiology, 291(2), H570-H580. doi:10.1152/ajpheart.01288.2005 | es_ES |
| dc.description.references | Xie, Y., Sato, D., Garfinkel, A., Qu, Z., & Weiss, J. N. (2010). So Little Source, So Much Sink: Requirements for Afterdepolarizations to Propagate in Tissue. Biophysical Journal, 99(5), 1408-1415. doi:10.1016/j.bpj.2010.06.042 | es_ES |
| dc.description.references | Yan, G.-X., Lankipalli, R. S., Burke, J. F., Musco, S., & Kowey, P. R. (2003). Ventricular repolarization components on the electrocardiogram. Journal of the American College of Cardiology, 42(3), 401-409. doi:10.1016/s0735-1097(03)00713-7 | es_ES |
| dc.description.references | Yang, T., Chun, Y. W., Stroud, D. M., Mosley, J. D., Knollmann, B. C., Hong, C., & Roden, D. M. (2014). Screening for Acute I Kr Block Is Insufficient to Detect Torsades de Pointes Liability. Circulation, 130(3), 224-234. doi:10.1161/circulationaha.113.007765 | es_ES |
| dc.description.references | Yang, P.-C., Song, Y., Giles, W. R., Horvath, B., Chen-Izu, Y., Belardinelli, L., … Clancy, C. E. (2015). A computational modelling approach combined with cellular electrophysiology data provides insights into the therapeutic benefit of targeting the late Na+current. The Journal of Physiology, 593(6), 1429-1442. doi:10.1113/jphysiol.2014.279554 | es_ES |
| dc.description.references | Yu, H., McKinnon, D., Dixon, J. E., Gao, J., Wymore, R., Cohen, I. S., … Rosen, M. R. (1999). Transient Outward Current, I to1 , Is Altered in Cardiac Memory. Circulation, 99(14), 1898-1905. doi:10.1161/01.cir.99.14.1898 | es_ES |
| dc.description.references | Zaniboni, M. (2011). 3D current–voltage–time surfaces unveil critical repolarization differences underlying similar cardiac action potentials: A model study. Mathematical Biosciences, 233(2), 98-110. doi:10.1016/j.mbs.2011.06.008 | es_ES |
| dc.description.references | Zaniboni, M. (2012). Late Phase of Repolarization is Autoregenerative and Scales Linearly with Action Potential Duration in Mammals Ventricular Myocytes: A Model Study. IEEE Transactions on Biomedical Engineering, 59(1), 226-233. doi:10.1109/tbme.2011.2170987 | es_ES |
| dc.description.references | Zaniboni, M., Pollard, A. E., Yang, L., & Spitzer, K. W. (2000). Beat-to-beat repolarization variability in ventricular myocytes and its suppression by electrical coupling. American Journal of Physiology-Heart and Circulatory Physiology, 278(3), H677-H687. doi:10.1152/ajpheart.2000.278.3.h677 | es_ES |
| dc.description.references | Zhao, Z., Xie, Y., Wen, H., Xiao, D., Allen, C., Fefelova, N., … Xie, L.-H. (2012). Role of the transient outward potassium current in the genesis of early afterdepolarizations in cardiac cells. Cardiovascular Research, 95(3), 308-316. doi:10.1093/cvr/cvs183 | es_ES |
| dc.description.references | Zhou, Q., Bett, G. C. L., & Rasmusson, R. L. (2012). Markov Models of Use-Dependence and Reverse Use-Dependence during the Mouse Cardiac Action Potential. PLoS ONE, 7(8), e42295. doi:10.1371/journal.pone.0042295 | es_ES |